You’ve probably heard about the debate surrounding the use of standing desks and their impact on your vein health. Do standing desk ergonomics cause varicose veins? In an increasingly health-conscious world, it’s essential to separate fact from fiction and make informed decisions about your workplace setup.
Standing desks alone don’t cause varicose veins; the way you use them matters for vein health. Maintaining good posture, taking regular breaks, and balancing sitting and standing can help mitigate any potential negative effects on your legs.
Curious? Keep reading to gain valuable insights and practical tips to keep your veins happy and healthy.
Understanding Varicose Veins
Before we dive deeper into the world of varicose veins, let’s clear up a common confusion – the difference between spider veins and varicose veins. Spider veins and varicose veins may both involve visible veins on the legs, but they are distinct in several ways.
To help you understand varicose veins better, here’s a video you can use as reference:
Spider veins, as the name suggests, resemble a spider’s web with their small, delicate, and often red or blue appearance. They tend to sit closer to the surface of the skin and are primarily a cosmetic concern. These veins are usually painless and don’t bulge out significantly.
On the other hand, varicose veins are larger, raised veins that can be twisted or swollen. Unlike spider veins, varicose veins can lead to discomfort and health complications. They often appear on the legs, and the symptoms associated with varicose veins can include aching, throbbing, or a heavy feeling in the legs. These symptoms may worsen after prolonged periods of standing or sitting.
Symptoms of Varicose Veins
Now that you can distinguish between spider veins and varicose veins, it’s important to recognize the symptoms of varicose veins to watch for.

Varicose veins can manifest in various ways, and the severity of symptoms can vary from person to person. Some common signs to be aware of include:
- Visible Veins: Enlarged, twisted, and bulging veins are the hallmark of varicose veins. They are often blue or dark purple and can appear knotted.
- Leg Discomfort: Individuals may experience a range of uncomfortable sensations in their legs. This can include a general aching or a throbbing pain. After long periods of standing or sitting, these sensations can intensify, leading to significant discomfort.
- Swelling: Poor circulation can lead to swelling, particularly in the lower legs, ankles, and calves. This swelling can be exacerbated towards the end of the day or after prolonged periods of inactivity.
- Skin Changes: The skin over or around varicose veins can undergo changes, such as darkening (hyperpigmentation), inflammation, or even eczema-like conditions. In advanced cases, the skin may become thin and prone to injury.
- Itching and Burning: Itching and burning sensations around the varicose veins are common. While these symptoms may seem superficial, they can be quite bothersome and may indicate underlying inflammation or changes in skin integrity due to the veins’ pressure.
Remember, the presence of these symptoms doesn’t necessarily mean you have varicose veins, but if you notice these signs, it’s advisable to consult a healthcare professional for a proper diagnosis and guidance on managing any potential vein issues.
Common Risk Factors for Developing Varicose Veins
Understanding the risk factors for developing varicose veins is crucial, as it can help you take preventive measures and make informed choices about your lifestyle and work environment. Here are some common risk factors:
- Age: As we age, our veins may lose their elasticity, making them more prone to developing varicose veins.
- Inactivity: A sedentary lifestyle, which involves long periods of sitting or standing without breaks, can contribute to poor blood circulation and increase the risk of vein issues.
- Obesity: Excess body weight puts added pressure on the veins in your legs, making it harder for blood to flow efficiently.
- Family and Personal Medical History: If you have a family history of varicose veins or have had them in the past, you may be at a higher risk.
- Pregnancy: Pregnancy can lead to increased pressure on the pelvic blood vessels, potentially causing varicose veins to develop.
- Gender: Women are more likely than men to develop varicose veins, partly due to hormonal changes and the strain of pregnancy.
Being aware of these risk factors can help you take proactive steps to minimize your chances of developing varicose veins. In the following sections, we’ll explore how lifestyle choices and workplace ergonomics can play a significant role in vein health.
Standing Desks: Boon or Bane for Vein Health?
Standing desks have gained immense popularity in recent years as a potential solution to the health risks associated with prolonged sitting. Many individuals have made the switch in an effort to promote better posture, reduce the risk of sore back pain, and enhance overall well-being. This trend has been driven by the belief that standing at work can be a healthier alternative to sitting for hours on end.

How Does Prolonged Standing Affect Leg Veins?
While the idea of standing desks promoting better posture and increased activity sounds promising, it’s crucial to understand how prolonged standing can affect your leg veins.
When you stand for extended periods, the blood in your veins must work against gravity to return to your heart. This can put added pressure on the veins in your legs, potentially causing blood to pool and veins to become engorged. As a result, you might experience symptoms such as aching, throbbing, or discomfort in your legs.
It’s important to note that the effects of prolonged standing on leg veins can vary from person to person, depending on factors like genetics, overall health, and how well you manage your time at the standing desk. While standing can engage your leg muscles and promote better circulation, excessive and uninterrupted standing may have adverse effects on your vein health.
Do Standing Desks Directly Contribute to Varicose Veins?
Now, let’s address a common question: do standing desks directly contribute to the development of varicose veins? The answer is not a simple yes or no. Standing desks themselves may not directly cause varicose veins, but they can play a role in their development if not used correctly. The key is finding the right balance.
According to the Center for Vein Restoration:
“Research suggests that patients with desk jobs should strive to strike a health balance between sitting, standing, and short walks throughout the work day. But above all it’s important to exercise, to get around 30 minutes of moderate activity for five days a week.”
Standing desks are most effective when they are used in conjunction with regular breaks and movements. Simply standing in one place for an extended period is not the ideal way to promote vein health. It’s essential to incorporate short breaks for sitting, walking, or even elevating your legs periodically to reduce the strain on your leg veins.
Now, if you already have varicose veins or related conditions, it’s important to consider how standing desks may impact your vein health, and to understand how long you should stand at a standing desk to avoid aggravating symptoms. For individuals with pre-existing vein issues, prolonged standing can exacerbate symptoms and discomfort.
It’s advisable to consult with a healthcare professional if you have varicose veins before making the switch to a standing desk. They can provide guidance on managing your condition while still benefiting from the ergonomic advantages of a standing desk. In the next sections, we’ll explore strategies to use standing desks effectively and mitigate potential vein-related concerns.
Debunking Common Myths about Varicose Veins and Standing Desks

Myth 1: Standing desks are the sole cause of varicose veins.
While prolonged standing can contribute to vein discomfort, it’s not the sole cause of varicose veins. Varicose veins are influenced by a combination of factors, including genetics, age, and lifestyle choices.
Myth 2: Only older people get varicose veins.
Varicose veins can affect individuals of all ages, not just older adults. While age is a risk factor, younger people can also develop varicose veins, especially if they have other contributing factors.
Myth 3: You can’t use a standing desk if you have varicose veins.
This is not necessarily true. With the right adjustments and habits, individuals with varicose veins can use standing desks effectively. It’s all about finding the right balance and incorporating proper ergonomics.
Myth 4: Only women get varicose veins.
While women are more commonly affected by varicose veins, men can develop them too. Hormonal changes, pregnancy, and genetics can make women more prone, but men should still be aware of the risk.
“They may be embarrassed to go for an evaluation, because they think of this as a vanity issue,” says Danielle Bajakian MD, a leading expert on vein disease at Columbia, “As a result, men minimize their symptoms, assuming that achy tired legs are the natural result of hard, physical work. They also assume that the pain is something they have to live with.”
Myth 5: Varicose veins are purely a cosmetic issue.
While varicose veins can be a cosmetic concern, they can also lead to discomfort, pain, and potentially more severe health issues if left untreated. It’s essential to address them, not just for appearance but also for overall health.
Myth 6: Varicose veins are untreatable.
This is far from the truth. Various treatment options are available, ranging from lifestyle changes and compression stockings to medical procedures. Consulting with a healthcare professional can help determine the best approach for your specific situation.
By dispelling these myths and clarifying misconceptions, we aim to provide you with accurate information about varicose veins and their relationship with standing desks. In the following sections, we’ll delve into prevention and management strategies, so you can make informed choices about your vein health.
Prevention and Management Strategies
Now that we’ve tackled the myths and misconceptions surrounding varicose veins and standing desks, it’s time to explore practical strategies for preventing and managing vein issues effectively.
Whether you’re looking to maintain healthy veins or seeking relief from existing symptoms, these strategies can make a significant difference in your vein health journey.

Use Compression Socks
Compression socks are a valuable tool in the management of varicose veins and can provide relief from discomfort. These socks are designed to apply graduated pressure to your legs, with the highest pressure at the ankle and gradually decreasing pressure as they move up the leg. This compression helps improve blood circulation by assisting the veins in pushing blood back towards the heart.
To make the most of compression socks, it’s essential to consult with a healthcare professional. They can assess your specific needs and recommend the appropriate level of compression and type of socks that will best address your vein issues. Wearing compression socks as recommended can be particularly beneficial if you spend long hours on your feet or have a history of varicose veins. It’s a simple and non-invasive solution that can significantly improve your vein health.
Prioritize Balancing Sitting and Standing at Work
Finding the right balance between sitting and standing at work is essential for maintaining good vein health. While standing desks have gained popularity, it’s crucial to avoid prolonged periods of standing without breaks. Excessive and prolonged standing can lead to blood pooling in your leg veins, increasing the risk of discomfort and vein-related issues.
To strike the right balance, consider the type of standing desk that allows you to switch between sitting and standing positions throughout the day. This flexibility allows you to relieve the pressure on your legs and promote better circulation. Additionally, incorporate short breaks into your work routine. Stand up, walk around, and perform simple leg stretches to keep your leg muscles engaged and the blood flowing. These breaks not only benefit your veins but also help prevent other posture-related discomforts.
It’s also important to pay attention to ergonomics. Ensure that your workstation is set up correctly to support good posture and minimize strain on your legs and back. The goal is to create a comfortable and healthy work environment that takes into account both sitting and standing.
Take Frequent Breaks and Leg Elevation
Taking regular breaks and elevating your legs can be a game-changer when it comes to vein health. Sitting or standing for prolonged periods can cause blood to accumulate in your leg veins, potentially leading to discomfort and swelling. To combat this, make it a habit to take short breaks throughout your workday.
During breaks, walk around and engage your leg muscles. This simple movement helps stimulate blood flow and reduces the risk of blood pooling in your leg veins. Additionally, whenever you have the opportunity, elevate your legs above heart level. This can be as simple as propping your legs up on an ergonomic chair or footrest for a few minutes. Elevating your legs helps gravity assist in returning blood to your heart, reducing pressure on your leg veins.
Incorporate Regular Exercise
Regular exercise, with a focus on walking, can be a powerful tool in the management of varicose veins. When you walk, the rhythmic contraction of your leg muscles helps pump blood back towards your heart, reducing the risk of blood pooling in your veins. This improved circulation not only lessens the chance of developing varicose veins but also provides relief for those already experiencing symptoms.
Incorporating daily walks into your routine doesn’t require a significant time commitment. Even short, brisk walks can have a positive impact on your vein health. Consider taking breaks during your workday to stretch your legs and go for a brief stroll. Additionally, activities like swimming and cycling are excellent options for those looking to engage in low-impact exercises that promote healthy blood flow in the legs.
Maintain a Healthy BMI and Stay Hydrated
Maintaining a healthy body mass index (BMI) is crucial for preserving vein health. Carrying excess weight places additional pressure on the veins in your legs, making them work harder to return blood to your heart. This increased strain can contribute to the development of varicose veins or exacerbate existing ones. By maintaining a healthy weight through a balanced diet and regular exercise, you reduce the burden on your leg veins and decrease the risk of vein-related issues.
In addition to managing your weight, staying adequately hydrated is key to promoting vein health. Proper hydration ensures that your blood maintains an appropriate viscosity, allowing it to flow smoothly through your veins. Dehydration can lead to thicker blood, making it more difficult for your veins to circulate blood effectively. Drinking enough water throughout the day is a simple yet effective way to support healthy blood circulation and reduce the likelihood of discomfort associated with varicose veins.
Choose Proper Clothing and Footwear
Your clothing and footwear choices can make a significant difference in promoting healthy circulation and reducing strain on your leg veins. Opt for loose-fitting, comfortable clothing that doesn’t constrict blood flow. Tight garments, especially around the waist and thighs, can impede proper circulation and contribute to vein discomfort.
When it comes to footwear, prioritize shoes that offer adequate support and cushioning. Properly fitting shoes with good arch support can help reduce the strain on your legs and veins, especially if you spend long hours standing or walking. Avoid high heels for extended periods, as they can negatively affect your posture and leg circulation. Choosing footwear that promotes comfort and maintains good circulation is a practical step towards better vein health. By considering these clothing and footwear considerations, you can make choices that contribute to the overall well-being of your legs and veins.
Potential Complications of Varicose Veins
While varicose veins may initially seem like a cosmetic concern or a minor discomfort, it’s essential to understand the potential complications that can arise if left unattended. These complications can have more severe consequences and underscore the importance of proactive vein health management. Let’s explore some of these complications and why early medical intervention is crucial.

Blood Clot
Another potential complication is the formation of blood clots within the varicose veins, a condition known as superficial thrombophlebitis. While these blood clots are usually not life-threatening, they can cause localized pain and inflammation. However, if the blood clot extends into deeper veins, it can lead to a more serious condition called deep vein thrombosis (DVT), which carries a risk of pulmonary embolism—a potentially life-threatening condition where the clot travels to the lungs.
Ulcer
One such complication is the development of venous ulcers. These ulcers are open sores that typically form near the ankles. They result from increased pressure and poor blood circulation in the affected veins. Venous ulcers can be painful, slow to heal, and prone to infection, significantly impacting your quality of life.
Bleeding
Additionally, varicose veins can be prone to bleeding, especially if the skin over them becomes thin and fragile. Even minor injuries or bumps can lead to bleeding episodes that may be challenging to control. While the bleeding itself is not typically life-threatening, it underscores the importance of addressing varicose veins to prevent such incidents.
Importance of Early Medical Intervention
Early medical intervention is crucial in managing varicose veins and preventing complications. If you experience symptoms like pain, swelling, or skin changes in the areas with varicose veins, it’s essential to seek professional medical advice promptly. Venous ulcers, blood clots, and bleeding episodes can often be prevented or managed effectively with timely medical attention.
Medical interventions may include minimally invasive procedures like endovenous laser treatment (EVLT), radio frequency ablation (RFA), or sclerotherapy. These procedures are designed to close off the problematic veins, redirecting blood flow to healthier ones. Additionally, lifestyle changes, such as regular exercise, elevation, and the use of compression stockings, can complement medical treatment and help prevent complications.
Ergonomic Tips for Using Standing Desks and Maintaining Vein Health
When using a standing desk, it’s essential to ensure that your desk setup promotes good vein health.
First, adjust the height of your standing desk so that your elbows are at a 90-degree angle when typing, and your monitor is at eye level. This helps maintain a neutral wrist and neck position, reducing the strain on your upper body.
Invest in an ergonomic anti-fatigue mat to reduce pressure on your feet and legs when standing for extended periods.
Wear comfortable, supportive shoes that provide adequate cushioning to reduce strain on your legs and promote proper circulation.
Additionally, make sure to choose an ideal desk size for optimal comfort, consider using a footrest to shift your weight between legs periodically.
Incorporating Movement and Posture Changes to Minimize Vein Stress
To minimize stress on your veins, incorporate movement into your work routine. Even at a standing desk, avoid static positions for too long.
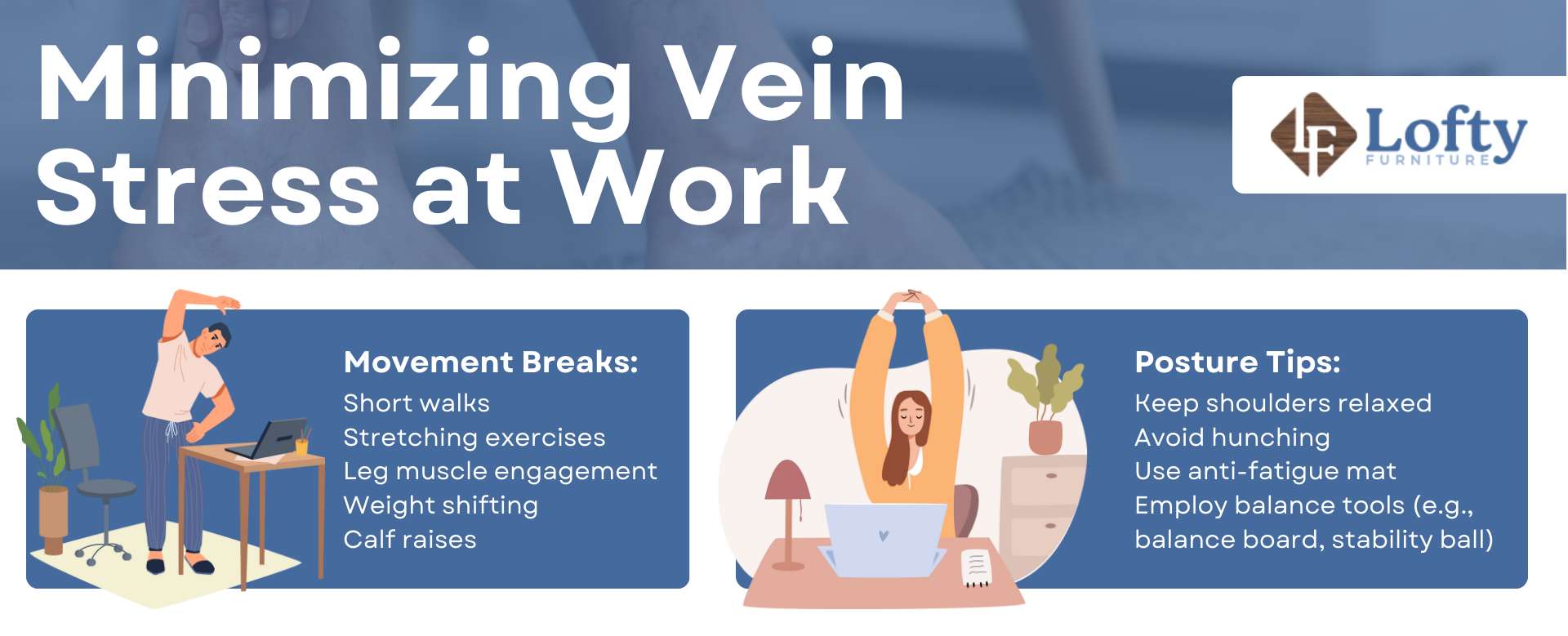
Take short breaks to walk around, stretch, and engage your leg muscles. Shift your weight from one leg to the other, and consider doing calf raises or gentle leg exercises to encourage blood flow.
Maintaining good posture is equally important. Keep your shoulders relaxed, and avoid hunching over your desk. Use an anti-fatigue mat to cushion your feet and reduce strain on your legs. If possible, use a balance board, standing desk treadmill, or stability ball to encourage subtle movements while standing, promoting circulation and preventing vein discomfort.
The Impact of Standing Desk Design on Vein Health
The design of your standing desk can significantly impact your vein health. Consider electric standing desks that offer height adjustment, allowing you to easily switch between sitting and standing positions. Look for features like a memory function that allows you to save preferred desk heights for convenience.
Additionally, the workspace and desk layout matters. Ensure that essential items like your keyboard, mouse, and monitor are within easy reach to avoid excessive reaching or bending. Proper cable management can prevent tripping hazards and clutter under your desk, creating a safer and more comfortable environment.
Conclusion
In the quest to understand the relationship between standing desks and varicose veins, it’s clear that the story is not black and white. While standing desks have gained popularity as a solution to the perils of prolonged sitting, their impact on vein health is nuanced. They can be a boon when used correctly, promoting better posture and movement, but a potential bane if overused without breaks and proper ergonomics.
The key takeaway is that varicose veins are influenced by a combination of factors, including genetics, age, lifestyle, and workplace habits. While standing desks may not directly cause varicose veins, they can play a role in their development or exacerbation if not used mindfully. The importance of finding the right balance between sitting and standing, taking regular breaks, and incorporating ergonomic principles into your workspace cannot be overstated.
Concerned about standing desk use and circulation? Stay active while you work!
Check out our Walking Pads & Treadmills to keep your legs moving and support healthy circulation.
